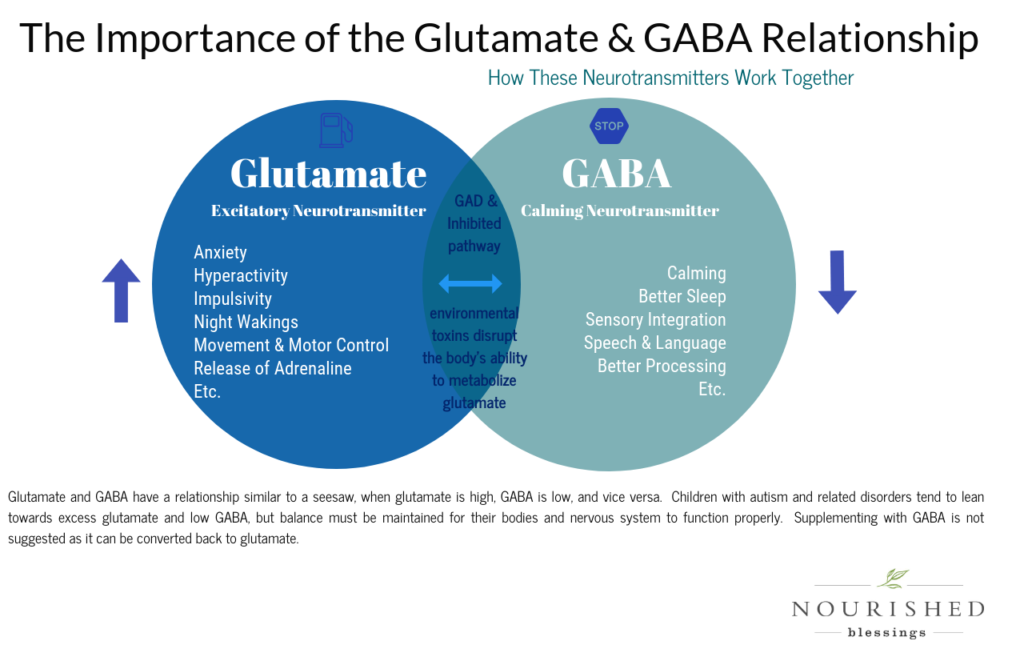
Glutamate is also the most abundant neurotransmitter, responsible for regulating over 50% of the nervous system, including the sensory system. Glutamate is considered to be an excitatory neurotransmitter, which means it excites or stimulates nerve cells located throughout the nervous system and facilitates the transmission of messages. The excitatory pathway is responsible for a wide variety of functions like the release of adrenaline, the control of movement and motor systems, learning, memory, and the expression of thought. It works in tandem with the inhibitory neurotransmitter GABA (gamma-aminobutyric acid), which calms and relaxes nerve cells and impedes the transmission of messages. GABA is also imperative for sensory integration, calming, mood/stress regulation, sleep, speech, and language. Glutamate and GABA have a relationship similar to a seesaw when glutamate is high, GABA is low, and vice versa. Glutamate and GABA need to be balanced.
When excitatory neurotransmitters (remember, glutamate is the most abundant excitatory neurotransmitter) acts without an inhibiting system (ie GABA), it results in a laundry list of unwanted symptoms and pain. Glutamate is the main neurotransmitter associated with the sensation of pain. – (Fein A. Nociceptors and the perception of pain. http://cell.uchc.edu/pdf/fein/nociceptors_fein_2012.pdf. Accessed July 21, 2020) Because of this, glutamate receptor antagonists and GABA receptor agonists are commonly used to reduce the sensation of pain. Unfortunately, interfering with these neurotransmitters artificially can further disrupt the delicate balance of these neurotransmitters and further exasperate the issues in the long run.
- Here is a fantastic podcast by the neuroscientist Dr. Kathleen Holton on the role of dietary glutamate in chronic pain.
- In this study, only MSG additives were removed; gluten, dairy, and soy were not removed. “This pilot data suggests an abnormally high prevalence of pain in Meru, Kenya, and that MSG intake, combined with dehydration, may be contributing to chronic widespread pain in this region. Improvement was defined as ≥30% reduction in pain impact score.” (Holton K. Dietary Correlates of Chronic Widespread Pain in Meru, Kenya. Nutrition, Volume 53, September 2018, Pages 14-19)
- “Among the neurotransmitters involved in pain transmission from the periphery to the brain, glutamate has a leading role. Glutamate is also involved in central sensitization, which is associated with chronic pain.” – (Pereira V. Emerging Trends in Pain Modulation by Metabotropic Glutamate Receptors Front Mol Neurosci. 2018; 11: 464. Accessed July 21, 2020)
- “Glutamate and glutamate receptors are also located in areas of the brain, spinal cord, and periphery that are involved in pain sensation and transmission. Not surprisingly, glutamate receptors have been an attractive target for new pain therapies. However, their widespread distribution and array of function has often resulted in drugs targeting these sites having undesirable side-effects.”- (Wozinak K.M. The role of glutamate signaling in pain processes and its regulation by GCP II inhibition, Curr Med Chem 2012;19(9):1323-34 Accessed July 21, 2020)
- “Glutamatergic mechanisms are implicated in acute and chronic pain, and there is a great diversity of glutamate receptors that can be used as targets for novel analgesics. Some approaches, e.g. NMDA receptor antagonism, have been validated clinically, however, the central side-effects have remained the main problem with most compounds. “- (Chizh, B. Novel approaches to targeting glutamate receptors for the treatment of chronic pain: Review article. Amino Acids 23, 169–176 (2002). https://doi.org/10.1007/s00726-001-0124-4)
-
“A lack of inhibition, particularly that mediated by gamma-amino butyric acid (GABA), the main inhibitory transmitter of the central nervous system (CNS), is responsible for many pain states. Until recently, few GABA acting drugs were available and were prescribed mostly for relieving muscle spasms, anxiety and epilepsy, but rarely for pain. The basic metabolic pathway of GABA is well known and we are now beginning to understand the function of this neurotransmitter in the complex circuitry underlying pain, especially in the context of nerve injury” -(Jasmin L. GABA Puts a Stop to Pain. Curr Drug Targets CSN Neural Disord 2004 Dec;3(6):487-505.)
Why Is This Important?
Because, glutamate is also the most abundant neurotransmitter, responsible for regulating over 50% of the nervous system. It is classified as an excitatory neurotransmitter, which means it excites or stimulates nerve cells located throughout the nervous system. Glutamate also has the ability to regulate other neurotransmitters, dopamine, serotonin and GABA are great examples. When glutamate is in excess it is extremely toxic to the brain and nervous system. It can become so excitatory, it is considered a excitotoxin, which means that it overstimulates brain cells to the point of killing them or damaging them enough to cause severe mitochondrial dysfunction (associated with low muscle tone) and neurological inflammation. Excess glutamate is believed to be involved in a variety of neurological and neurodegenerative disorders including autism, obsessive compulsive disorders, hyperactivity disorders, complex motor stereotypes, tics, insomnia, anxiety disorders, seizures, sensory processing disorder, addiction, depression, chronic fatigue, PANS, PANDAS, Alzheimers, and so on. Excess glutamate also impairs methylation and depletes glutathione levels, which are vital for detoxification, controlling inflammation and gut health. Working to lower glutamate/inflammation and balance GABA, is key to improving overall health.
Obviously diet (REID) is one of the most important if not, the most important step in lowering glutamate. However, this natural option may prove beneficial in helping when experiencing a peak of symptoms related to high glutamate and neurological inflammation, i.e. following consumption of a high glutamate food, trauma or a “flare” from PANS (pediatric autoimmune neuropsychiatric disorder) or PANDAS (pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections). Additionally, working to lower inflammation/glutamate by treating underlying sources inflammation (metals, microbial imbalances, parasites, microglial activation, poor detoxification pathways, various toxins, etc.) will also be hugely beneficial. We’ve personally found homeopathy to be great for this.
I do not have personal experience with all options mentioned in the “Lowering Glutamate” page, nor would I recommend all of them (especially the pharmaceutical options). You will want to read the comments as some of the items used to temporarily lower glutamate, can actually work to increase glutamate/glutamate sensitivity over time.
The information shared within this blog has been gathered by a mother, not a physician, and should not act as medical advice. Under no circumstances shall I, or any contributors and affiliates of the blog, be responsible for damages arising from use of the blog.